Guide to Acne Scar Types and Classifications
Acne Scar Types Infographics

Cost
$450 to $1200
Procedure time
30 to 90 Minutes
Results Duration
Can Be Permanent
Level of Discomfort
Moderate to high
Hypertrophic and Keloid Scars (Raised Scars)
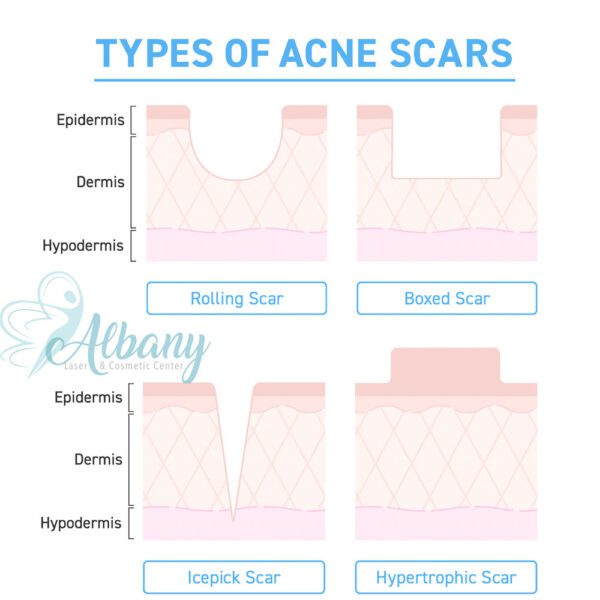
Types of Acne Scars

Here’s an overview of what you might expect with each scar type:
Atrophic Scars (Indented)
These scars result from tissue loss and appear as depressions in the skin. They are commonly seen after severe acne and are further divided into three subtypes:
- Ice Pick Scars: Small but deep, these scars resemble tiny punctures, giving the skin a pitted look. They may take longer to heal and typically require advanced treatments like microneedling or chemical peels.
- Boxcar Scars: Broad depressions with well-defined edges, these scars often occur on the cheeks and jawline. While shallow boxcar scars may respond well to laser resurfacing, deeper ones need more intensive treatments.
- Rolling Scars: These scars create wave-like patterns across the skin, caused by fibrous bands pulling the surface down. Subcision or dermal fillers are often used to smooth out these scars
Hypertrophic Scars (Raised)
Hypertrophic and Keloid Scars: Raised, firm scars caused by excessive collagen production. They are more common on the chest, back, and shoulders and often require steroid injections or laser therapy. These scars form due to excess collagen production.
- Hypertrophic scars stay within the boundary of the original acne site.
- keloid scars extend beyond it, forming large, raised areas. These scars are more common in individuals with darker skin tones.
Scar Classification and Types
What are the different types of scars?
There are several types of scars, each with unique characteristics:
- Atrophic Scars:
- Description: Depressed or sunken scars caused by tissue loss.
- Examples: Acne scars, chickenpox scars.
- Treatment: Microneedling, chemical peels, or laser resurfacing (e.g., Fraxel).
- Hypertrophic Scars:
- Description: Raised, thickened scars that remain within the wound boundary.
- Common Causes: Surgical scars, burns, or injuries.
- Treatment: Steroid injections, silicone sheets, or laser treatments (e.g., pulsed-dye laser).
- Keloid Scars:
- Description: Raised and larger than the original wound; can grow beyond the wound’s borders.
- Common Causes: Genetic predisposition, often seen in darker skin tones.
- Treatment: Steroid injections, cryotherapy, surgical excision, or laser therapy.
- Contracture Scars:
- Description: Tight, thickened scars that occur when the skin pulls together, often restricting movement.
- Common Causes: Burns.
- Treatment: Physical therapy, surgery, or skin grafts.
- Hyperpigmented Scars:
- Description: Dark discoloration that remains after an injury or acne heals.
- Common Causes: Inflammatory conditions or trauma, especially in darker skin.
- Treatment: Topical lightening agents (e.g., hydroquinone), chemical peels, or laser therapy.
How do I know which treatment is right for my scar type?
- Atrophic Scars:
- Best suited for microneedling, subcision, or CO2 laser to promote collagen production.
- Hypertrophic Scars:
- Steroid injections can reduce thickness. Silicone sheets help flatten and soften the scar.
- Keloids:
- Cryotherapy or a combination of steroid injections and laser treatments can reduce size and prevent recurrence.
- Contracture Scars:
- Surgical options and physical therapy are often needed to restore movement.
- Hyperpigmentation:
- Chemical peels or topical products like retinoids and vitamin C serums work well to fade discoloration.
What factors influence scar formation?
Several factors impact the type and appearance of scars:
- Genetics: People with a family history of keloids are more likely to develop them.
- Skin tone: Darker skin tones are more prone to hyperpigmentation and keloids.
- Location: Scars on areas with more tension (like the chest or shoulders) may become hypertrophic or keloid.
- Wound care: Proper wound management (e.g., keeping it clean and moist) reduces the risk of scarring.
How long does it take for a scar to fully heal?
- Initial healing: Takes around 2 to 6 weeks for the wound to close and the scar to form.
- Maturation phase: Can take 3 months to 1 year, as collagen production remodels the scar tissue.
- Full scar improvement: Some treatments may take 6 months to 1 year to show final results, especially with laser or microneedling.
Can all scars be removed completely?
- Most scars cannot be fully erased, but their appearance can be significantly improved.
- Treatment goals focus on reducing the scar’s visibility, evening out skin texture, and minimizing pigmentation changes.
What is the difference between hyperpigmentation and a scar?
- Hyperpigmentation refers to discoloration caused by excess melanin production following an injury. It is not a true scar and can fade over time with proper care.
- Scars involve structural damage to the skin (e.g., raised or depressed areas) and may require more intensive treatments to correct.